What is Posttraumatic Stress Disorder (PTSD)?
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event, series of events or set of circumstances.
A traumatic incident, series of events, or set of circumstances may cause a person to develop posttraumatic stress disorder (PTSD), a mental disease. This could be perceived by a person as being emotionally, physically, or even life-threatening, which could have an impact on their mental, physical, social, and/or spiritual health. Examples include violent acts against personal partners, serious accidents, terrorist attacks, war and conflict, rape, and sexual assault, as well as historical trauma.
In the past, PTSD has gone by a variety of labels, including "shell shock" during World War I and "combat fatigue" following World War II, but it does not only affect combat veterans. Any person, of any race, nation, or culture, and at any age, may experience PTSD. Every year, 3.5 percent of adult Americans suffer from PTSD. For adolescents aged 13 to 18, the lifetime prevalence of PTSD is 8%. Approximately one in eleven persons may receive a PTSD diagnosis over their lifetime. PTSD is twice as common in women as it is in men. In comparison to non-Latino whites, PTSD rates are greater among three ethnic groups: U.S. Latinos, African Americans, and Native Americans/Alaska Natives.
Long after the horrific incident has passed, people with PTSD continue to endure intense, unsettling thoughts and sensations related to their experience. Flashbacks or dreams may cause them to relive the incident, they may experience sadness, fear, or rage, and they may feel distant or estranged from other people. A loud noise or an unintentional touch can trigger significant negative reactions in those with PTSD, who may avoid circumstances or people who remind them of the traumatic occurrence.
It takes exposure to a distressing traumatic experience for PTSD to be diagnosed. Directly experiencing an event, seeing a terrible event happen to someone else, or finding out that a traumatic event occurred to a close family member or acquaintance are all examples of exposure. It may also happen as a result of frequent exposure to gruesome traumatizing information, such as when police officers are exposed to child abuse case specifics.
Symptoms and Diagnosis
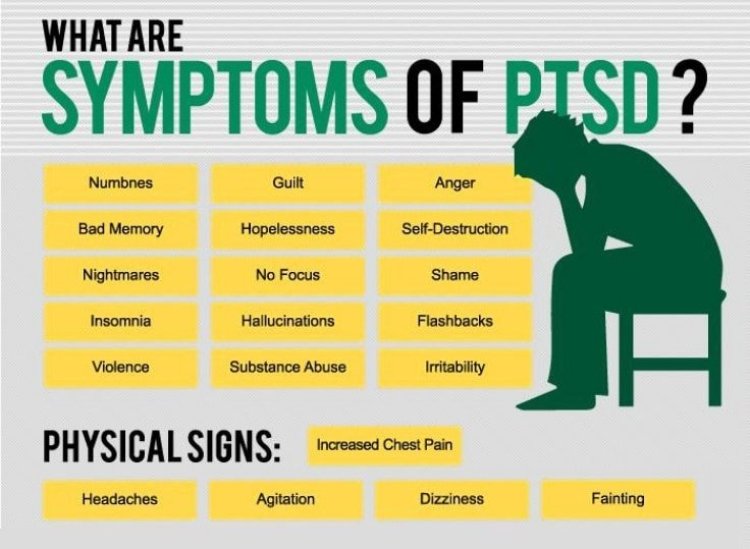
PTSD symptoms can be categorized into the following four groups. The severity of particular symptoms can vary.
Intrusion: Persistent, unwanted thoughts, upsetting nightmares, or flashbacks to the traumatic incident are examples of intrusive thoughts. People who experience flashbacks sometimes feel as though they are witnessing or reliving the painful event.
Avoidance: Steer clear of people, places, things, activities, and situations that can bring back unpleasant memories as part of your avoidance strategy. People could make an effort to forget or stop thinking about the terrible experience. They can be reluctant to discuss what occurred or how they feel about it.
Changes in cognition and mood include the inability to recall crucial details of the traumatic event, negative emotions leading to persistent and distorted beliefs about oneself or others (e.g., "I am bad," "No one can be trusted"), distorted ideas about the cause or consequences of the event leading to incorrectly placing blame on oneself or others, much less interest in once-enjoyed activities, and a detached or estranged feeling.
Changes in arousal and reactivity include irritability and angry outbursts, reckless or self-destructive behavior, being suspiciously overly aware of one's surroundings, being easily startled, having trouble concentrating, or having trouble sleeping.
In the days following a stressful occurrence, many people are affected by symptoms resembling those mentioned above. However, symptoms must persist for more than a month and must cause the person severe discomfort or difficulty with everyday functioning in order for PTSD to be diagnosed. The majority of people experience symptoms within three months of the event, but they can also arise later and last for weeks, months, or even years. PTSD frequently co-occurs with other closely related diseases like depression, substance abuse, memory issues, and other issues with physical and mental health.
Related Conditions
Acute Stress Disorder
Similar to PTSD, acute stress disorder also results from a traumatic experience and exhibits similar symptoms. But the signs show up three days to a month after the incident. Acute stress disorder patients may experience flashbacks or dreams, relive the event, and feel numb or distant from themselves. These symptoms significantly disrupt their daily lives and cause them great distress. Acute stress disorder leads to PTSD in about 50% of cases. 19% to 50% of people who encounter interpersonal violence (such as rape, assault, and intimate partner violence) have been diagnosed with acute stress disorder.
Cognitive behavior therapy, for example, can help regulate symptoms and stop them from getting worse and turning into PTSD. SSRI antidepressants are one type of medication that can help with the symptoms.
Adjustment Disorder
A stressful life event (or events) can trigger adjustment disorder. In general, a person's emotional or behavioral symptoms in response to a stressor are more severe or intense than what may be expected given the nature of the incident that occurred.
Feeling tense, depressed, or despairing; withdrawing from others; behaving irrationally or impulsively; or physical signs such as tremors, palpitations, and headaches. The symptoms significantly impair someone's ability to function in important spheres of their life, such as at job, school, or in social situations. Within three months of a stressful event, symptoms of adjustment problems appear, and they remain for no more than six months after the event has passed or its effects have subsided.
A breakdown in a love relationship is an example of a single stressor, but there could be multiple events that have a cumulative effect. Stressors can occur repeatedly or continuously (for example, a chronic sickness that is becoming more and more incapacitating). A single person, an entire family, or a larger group or community (for instance, in the event of a natural disaster) may be affected by a stressor.
An estimated 5% to 20% of patients receiving outpatient mental health care have an adjustment disorder as their primary diagnosis. More than 15% of adults with cancer experienced adjustment disorder, according to a recent study. Psychotherapy is often used to treat it.
Disinhibited Social Engagement Disorder
Children with significant social neglect or deprivation before the age of two often develop disinhibited social engagement disorder. Similar to reactive attachment disorder, it can develop when kids lack the fundamental emotional requirements of affection, stimulation, and comfort or when frequent changes in caregivers (such frequent foster care transfers) make it difficult for them to establish enduring bonds.
A youngster with disinhibited social interaction disorder will act out with unfamiliar people in a way that is overly familiar or unsuitable for their culture. The child might, for instance, be willing to leave the house with an unknown adult with little to no hesitation. This disease frequently co-occurs with developmental abnormalities, including cognitive and language disabilities. There is evidence that the caliber of caregiving can influence how this condition develops. However, some kids may continue to experience symptoms well into puberty despite changes in the setting for providing care.
Disinhibited social interaction disorder is assumed to be uncommon, while its frequency is unknown. Most children who are maltreated severely never have the disorder. Working with caregivers to make sure the child has an emotionally accessible attachment figure is the most crucial aspect of treatment.
Reactive Attachment Disorder
Children who have suffered from significant social neglect or deprivation during their early years of life develop reactive attachment disorder. It can happen when kids lack the fundamental emotional requirements for solace, stimulation, and affection or when frequent caregiver changes (such frequent foster care transfers) hinder kids from developing enduring relationships.
Reactive attachment disorder causes children to emotionally distance themselves from their adult carers. They hardly ever seek the comfort, protection, or support of caretakers, or they do not take comfort when they are upset. They display little positive emotion in typical encounters with caretakers and may exhibit irrational fear or melancholy. The issues show up before age 5. Delays in cognitive and verbal development, in particular, frequently coexist with the illness.
Even among children who have been severely neglected, reactive attachment disorder is rare. In order to improve the bond between a kid and their primary caregivers, treatment entails a therapist working with the child's family.
Treatment
It's crucial to remember that not everyone who encounters trauma goes on to acquire post-traumatic stress disorder (PTSD), and not everyone with PTSD needs psychiatric care. Some people experience PTSD symptoms that gradually get better or go away. Others improve with the aid of their support network, which may include family, friends, or the clergy. However, many PTSD sufferers require medical attention to overcome their psychological discomfort, which can be severe and incapacitating. It's critical to keep in mind that trauma can cause serious distress. PTSD is treatable, and the distress is not the person's fault. A person has a better chance of recovering if they receive treatment sooner.
To assist people in recovering from PTSD, psychiatrists and other mental health specialists employ a variety of efficient (research-proven) techniques. PTSD can be effectively treated with medication and talk therapy (psychotherapy), according to evidence-based medicine.
Cognitive Behavioral Therapy
Cognitive behavior treatments (CBT) are a very effective subset of psychotherapy. Among the CBT techniques used to treat PTSD are cognitive processing treatment, prolonged exposure therapy, and stress inoculation therapy (detailed below).
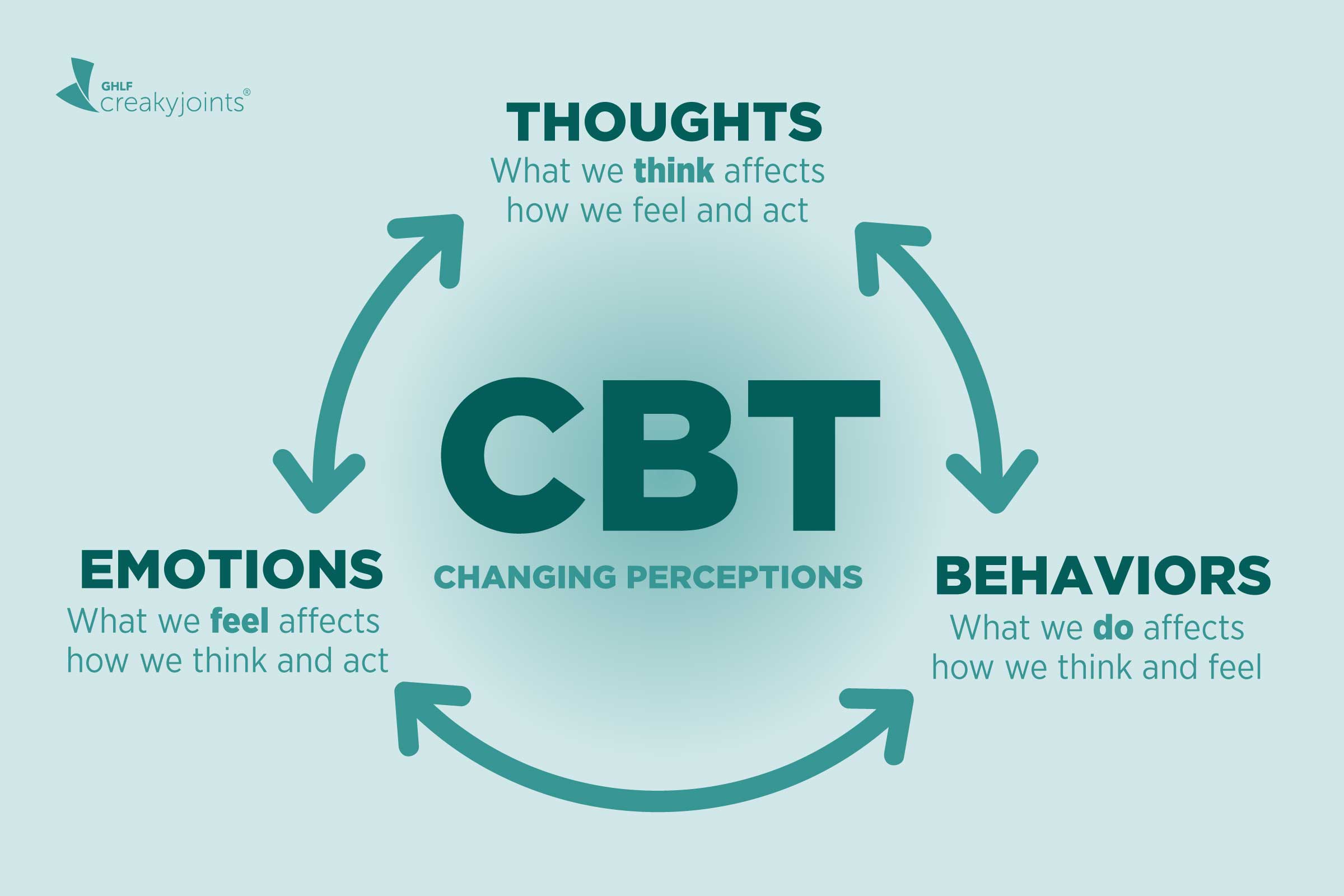
Cognitive Processing Therapy is an evidence-based, cognitive behavioral therapy designed specifically to treat PTSD and comorbid symptoms. It focuses on changing painful negative emotions (such as shame, guilt, etc.) and beliefs (such as “I have failed;” “the world is dangerous”) due to the trauma. Therapists help the person confront such distressing memories and emotions.
- Prolonged Exposure Therapy uses repeated, detailed imagining of the trauma or progressive exposures to symptom “triggers” in a safe, controlled way to help a person face and gain control of fear and distress and learn to cope. For example, virtual reality programs have been used to help war veterans with PTSD re-experience the battlefield in a controlled, therapeutic way.
- Trauma Focused Cognitive Behavioral Therapy is an evidence-based treatment model for children and adolescents that incorporates trauma-sensitive interventions with cognitive behavioral, family, and humanistic principles and techniques.
- Eye Movement Desensitization and Reprocessing for PTSD is a trauma-focused psychotherapy which is administered over approximately 3 months. This therapy helps a person to reprocess the memory of the trauma so that it is experienced in a different way. After a thorough history is taken and a treatment plan developed the therapist guides the patient through questions about the traumatic memory. Eye movements similar to those in REM sleep is recreated during a session by having the patient watch the therapist’s fingers go back and forth or by watching a light bar. The eye movements last for a brief time period and then stop. Experiences during a session may include changes in thoughts, images, and feelings. After repeated sessions the memory tends to change and is experienced in a less negative manner.
- Group therapy encourages survivors of similar traumatic events to share their experiences and reactions in a comfortable and non-judgmental setting. Group members help one another realize that many people would have responded the same way and felt the same emotions. Family therapy may also help because the behavior and distress of the person with PTSD can affect the entire family.
Other psychotherapies such as interpersonal, supportive and psychodynamic therapies focus on the emotional and interpersonal aspects of PTSD. These may be helpful for people who do not want to expose themselves to reminders of their traumas.
Medication
PTSD symptoms can be managed with the aid of medication. Additionally, the symptom relief that medicine offers enables many patients to engage in psychotherapy more productively.
The primary symptoms of PTSD are frequently treated with antidepressants, particularly SSRIs and SNRIs (selective serotonin re-uptake inhibitors and serotonin-norepinephrine re-uptake inhibitors). They may be utilized independently or in conjunction with other therapies such as psychotherapy.
Other drugs may be used to treat PTSD-related nightmares and sleep issues, as well as to reduce anxiety and physical discomfort.
Other Treatments
PTSD patients are also increasingly receiving aid from other therapies, such as complementary and alternative medicine. In comparison to psychotherapy, these methods offer treatment outside of the typical mental health clinic and could include less talking and disclosure. Acupuncture, yoga, and animal-assisted therapy are a few examples.
Many PTSD sufferers find it extremely beneficial to talk about their experiences and feelings with other people who understand them, such as in a peer support group, in addition to receiving treatment.
References
- American Psychiatric Association. (2022). Trauma- and Stressor-Related Disorders. In Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.).
- Bichitra Nanda Patra and Siddharth Sarkar. Adjustment Disorder: Current Diagnostic Status. Indian J Psychol Med. 2013 Jan-Mar; 35(1): 4–9.
- Harvard Medical School. (2007). National Comorbidity Survey (NCS). (2017, August 21). Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort.
- National Library of Medicine: MedlinePlus. Adjustment Disorder.
- American Academy of Child and Adolescent Psychiatry. Facts for Families: Attachment Disorders.
- Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.>
- Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.